|
Getting your Trinity Audio player ready...
|
The Relationship Between Tension-Type Headaches and Migraine Headaches
Tension-type headaches (TTH) and migraine headaches are two of the most common forms of primary headaches, yet they differ in presentation, pathophysiology, and often, in the intensity of the pain. However, they share certain neurobiological pathways and physiological triggers that suggest a complex relationship between the two, where tension-type headaches may contribute to the onset or worsening of migraines and vice versa. Understanding the anatomy and physiology involved in these types of headaches provides valuable insight into how they interact and influence one another.
Anatomy and Physiology of Tension-Type Headaches and Migraine Headaches
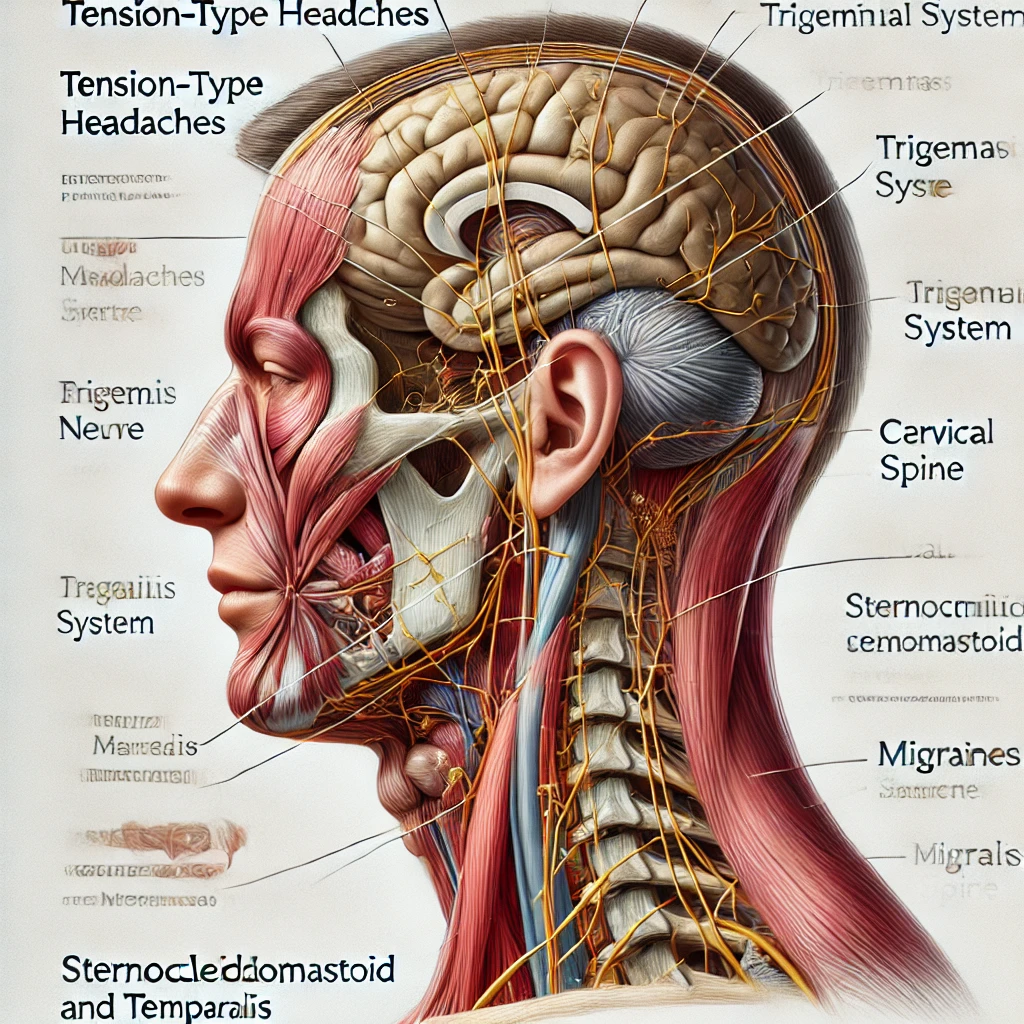
Tension-type headaches are often linked to muscular tension in the head, neck, and shoulders, involving the myofascial tissues and pericranial muscles (Lipton et al., 2001). This muscle tension may trigger central sensitization—an increased responsiveness of neurons in the central nervous system to stimuli, leading to pain. Anatomically, TTH is associated with structures like the trapezius, sternocleidomastoid, and temporalis muscles, which, when under prolonged tension, send nociceptive signals to the brainstem, where pain is processed (Ashina, 2002).
Migraine headaches, on the other hand, are believed to be associated with hyperexcitability of the brainstem and cortex. Migraines are also closely related to the trigeminovascular system, where the trigeminal nerve innervates blood vessels in the meninges, causing neurogenic inflammation and pain (Burstein et al., 2000). Activation of these structures leads to the release of pro-inflammatory neuropeptides, which can cause vasodilation and inflammation around the meninges, resulting in migraine pain (Edvinsson et al., 2019).
Mechanisms Linking Tension-Type Headaches to Migraine Headaches
Studies have shown that individuals with frequent TTH may have a heightened risk of developing migraines, likely due to shared pathways in pain processing. Both TTH and migraines involve central sensitization, where repeated episodes of TTH could prime the brain to respond more intensely to future pain stimuli. This effect is sometimes called the “kindling effect,” where frequent stimulation lowers the threshold for activating the trigeminovascular system, making an individual more susceptible to migraines (Ashina et al., 2017).
Moreover, sustained muscle tension in TTH could trigger the trigeminocervical complex (TCC), a critical area involved in the transmission of headache-related pain. The TCC integrates sensory information from the upper cervical spinal nerves and the trigeminal nerve, which play a key role in both tension and migraine headaches (Biondi, 2005). When TTH activates the TCC, it may initiate or worsen migraine symptoms through this shared anatomical structure.
Migraine Headaches Triggering Tension-Type Headaches
Conversely, migraines can also lead to TTH, particularly during the postdromal phase of a migraine. Known as “migraine hangover,” this phase is marked by fatigue, muscle pain, and lingering headache symptoms, which may present as a tension-type headache. Additionally, migraine-induced central sensitization can lead to persistent muscular tension in the pericranial muscles, causing tension-type pain even after the migraine episode resolves (Lipton et al., 2001).
Migraine-associated allodynia, a condition where normally non-painful stimuli become painful, also contributes to TTH. The sensitization of neurons in the trigeminovascular system and spinal cord can increase sensitivity to touch and pressure, leading to sustained tension in the head and neck muscles and the development of TTH in individuals with migraines (Burstein et al., 2000).
Clinical Implications and Management Strategies
The interplay between TTH and migraine headaches suggests that treating one type of headache could reduce the occurrence of the other. For instance, muscle relaxation techniques, biofeedback, and physical therapy for tension-type headache management may reduce the overall headache burden and lower the risk of migraine onset. Similarly, effective pharmacological management of migraines, including triptans and CGRP inhibitors, may reduce the frequency and severity of tension-type headaches by minimizing central sensitization (Ashina et al., 2017).
Mindfulness practices and stress-reduction strategies are also valuable, as both TTH and migraines can be exacerbated by psychological stress. Comprehensive headache management plans that address both types of headaches may therefore yield better outcomes, especially in patients with comorbid TTH and migraine (Edvinsson et al., 2019).
Conclusion
The relationship between tension-type headaches and migraine headaches is rooted in shared neurobiological and anatomical pathways. Through mechanisms like central sensitization, the trigeminocervical complex, and muscle tension, one type of headache can set the stage for the other, creating a cycle that can be challenging for patients and healthcare providers. Understanding these connections allows for more effective, holistic treatment strategies, aimed at reducing both TTH and migraine frequency and intensity.
References
- Ashina, M. (2002). Neurobiology of tension-type headache. Cephalalgia, 22(9), 701-721.
- Ashina, M., Katsarava, Z., & Buse, D. C. (2017). Migraine and tension-type headache: Prophylactic treatment strategies. The Journal of Headache and Pain, 18(1), 41.
- Biondi, D. M. (2005). Cervicogenic headache: A review of diagnostic and treatment strategies. The Journal of the American Osteopathic Association, 105(4_suppl), 16S-22S.
- Burstein, R., Collins, B., & Jakubowski, M. (2000). Defeating migraine pain with triptans: A race against the development of cutaneous allodynia. Annals of Neurology, 47(4), 377-385.
- Edvinsson, L., Villalón, C. M., & MaassenVanDenBrink, A. (2019). Basic mechanisms of migraine and its acute treatment. Pharmacology & Therapeutics, 193, 17-37.
- Lipton, R. B., Stewart, W. F., & Scher, A. I. (2001). Epidemiology and economic impact of migraine. Current Neurology and Neuroscience Reports, 1(1), 109-115.
