|
Getting your Trinity Audio player ready...
|
Understanding Concussions: Symptoms, Assessment, and Contraindications in Musculoskeletal Care
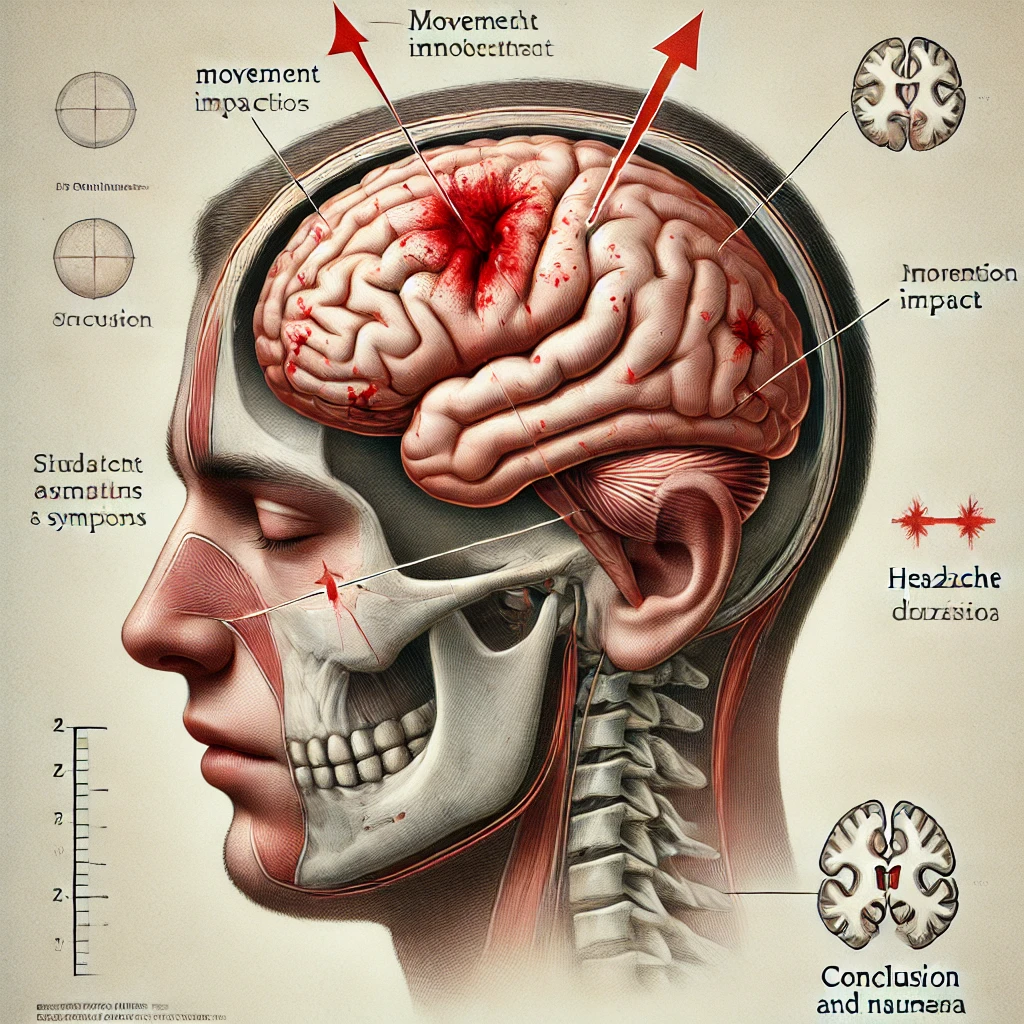
Concussions, classified as mild traumatic brain injuries (mTBIs), result from a direct or indirect impact to the head or body that causes brain movement within the skull (McCrory et al., 2017). Recognizing and managing concussion effectively is essential in preventing long-term health impacts, especially in the context of musculoskeletal and rehabilitative care. This article discusses the progression of concussion symptoms, red flags, assessment questionnaires, contraindications for treatment by physiotherapists and chiropractors, and relevant history and tests that help identify concussion.
Symptom Progression
Concussion symptoms can emerge immediately or gradually over several hours or days. They typically progress through three stages:
- Immediate Symptoms: These occur within minutes to hours post-injury and may include confusion, dizziness, nausea, and headaches (McCrory et al., 2017). Memory issues and attention deficits may also be present initially.
- Intermediate Symptoms: Within 24–48 hours, the patient may report persistent headache, sensitivity to light and noise, irritability, and sleep disturbances (Echemendia et al., 2017). Cognitive symptoms, such as difficulty concentrating and memory challenges, can intensify over time.
- Persistent Symptoms: In cases of prolonged recovery (often termed post-concussion syndrome), symptoms may persist beyond 3 months. These include prolonged cognitive issues, psychological symptoms such as depression or anxiety, and vestibular dysfunctions (Iverson et al., 2017).
Red Flags for Immediate Referral
Certain symptoms warrant urgent referral to emergency care, as they may suggest more severe brain injury. These include (McCrory et al., 2017):
- Worsening headache
- Repeated vomiting
- Seizures
- Slurred speech
- Weakness or numbness in extremities
- Confusion that worsens over time
Assessment Tools and Questionnaires
Several standardized tools can help assess and monitor concussion symptoms:
- SCAT5 (Sports Concussion Assessment Tool)
The SCAT5 is widely used in clinical settings to assess acute concussion. It evaluates symptoms, cognitive function, balance, and coordination, providing a baseline for tracking recovery (Davis et al., 2017). - ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing)
This computer-based test evaluates neurocognitive functions, such as memory, processing speed, and reaction time, and is commonly used in athletic populations (Schatz & Sandel, 2013). - Rivermead Post-Concussion Symptoms Questionnaire (RPQ)
The RPQ assesses the severity of symptoms over the recovery period and can track prolonged symptoms for post-concussion syndrome (King et al., 1995).
Contraindications for Physiotherapy and Chiropractic Treatment
Concussion patients should receive careful consideration when undergoing musculoskeletal or spinal treatments. Contraindications include:
- Manual cervical manipulations: High-velocity manipulations may exacerbate symptoms like dizziness, headache, and nausea and should be avoided in the acute phase post-concussion (Zhu et al., 2020).
- Vestibular interventions: Exercises that overstimulate the vestibular system may worsen symptoms in patients with vestibular dysfunction related to concussion (Ellis et al., 2015).
- Cervical traction or aggressive mobilizations: These may exacerbate symptoms in individuals with neck pain secondary to concussion or whiplash-associated disorders (McCrory et al., 2017).
Case History and Relevant Tests
An accurate case history and physical assessment are critical for concussion identification. Important history aspects include:
- Mechanism of Injury: Documenting the specific cause of injury, such as a fall or sports collision, and associated symptoms like confusion or amnesia is essential (Iverson et al., 2017).
- Symptom Onset and Progression: Understanding how quickly symptoms appeared and whether they worsened over time helps differentiate between concussion and other types of head trauma (Echemendia et al., 2017).
- Previous Head Injuries: Recurrent concussions increase the risk of prolonged symptoms and other complications (McCrory et al., 2017).
Orthopedic and Neurological Special Tests
Specific tests can help identify the presence of a concussion:
- Cervical Spine Assessment: Tenderness, restricted range of motion, or pain during cervical examination may indicate concurrent whiplash or soft tissue injury, which is common with concussions (Zhu et al., 2020).
- Balance and Coordination Tests: Tests such as the tandem gait test and Romberg test assess balance deficits related to concussion (Guskiewicz et al., 2001).
- Cranial Nerve Examination: Checking for visual changes (e.g., diplopia or photophobia), nystagmus, or vestibular signs can indicate neurological involvement post-concussion (McCrory et al., 2017).
Conclusion
Early identification and appropriate management of concussion are essential to minimize the risk of persistent symptoms. Practitioners must be vigilant for symptom progression and red flags, use validated assessment tools, and carefully avoid contraindicated treatments. A comprehensive history and examination, including orthopedic and neurological tests, further aid in diagnosing concussion accurately, allowing for timely intervention and referral when necessary.
References
- Davis, G. A., Ellenbogen, R., Bailes, J., et al. (2017). The 5th international conference on concussion in sport: Consensus statement. British Journal of Sports Medicine, 51(11), 838-847.
- Echemendia, R. J., Broglio, S. P., Davis, G. A., et al. (2017). What tests and measures should be included in a comprehensive concussion assessment? British Journal of Sports Medicine, 51(11), 847-851.
- Ellis, M. J., Leddy, J., Willer, B. (2015). Physiological, vestibulo-ocular, and cervicogenic post-concussion disorders: An evidence-based classification system with directions for treatment. Brain Injury, 29(2), 238-248.
- Guskiewicz, K. M., Ross, S. E., & Marshall, S. W. (2001). Postural stability and neuropsychological deficits after concussion in collegiate athletes. Journal of Athletic Training, 36(3), 263–273.
- Iverson, G. L., Gardner, A. J., Terry, D. P., et al. (2017). Predictors of clinical recovery from concussion: A systematic review. British Journal of Sports Medicine, 51(12), 941-948.
- King, N. S., Crawford, S., Wenden, F. J., et al. (1995). The Rivermead Post-Concussion Symptoms Questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. Journal of Neurology, 242(9), 587–592.
- McCrory, P., Meeuwisse, W., Dvorak, J., et al. (2017). Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. British Journal of Sports Medicine, 51(11), 838-847.
- Schatz, P., & Sandel, N. (2013). Sensitivity and specificity of the online version of ImPACT in high school and collegiate athletes. The American Journal of Sports Medicine, 41(2), 321-326.
- Zhu, F., Liu, Y., Zhao, W., et al. (2020). Manual therapy for cervical dizziness: A systematic review and meta-analysis. Frontiers in Neurology, 11, 560.
