|
Getting your Trinity Audio player ready...
|
Effectiveness of Extracorporeal Shock Wave Therapy (ESWT)
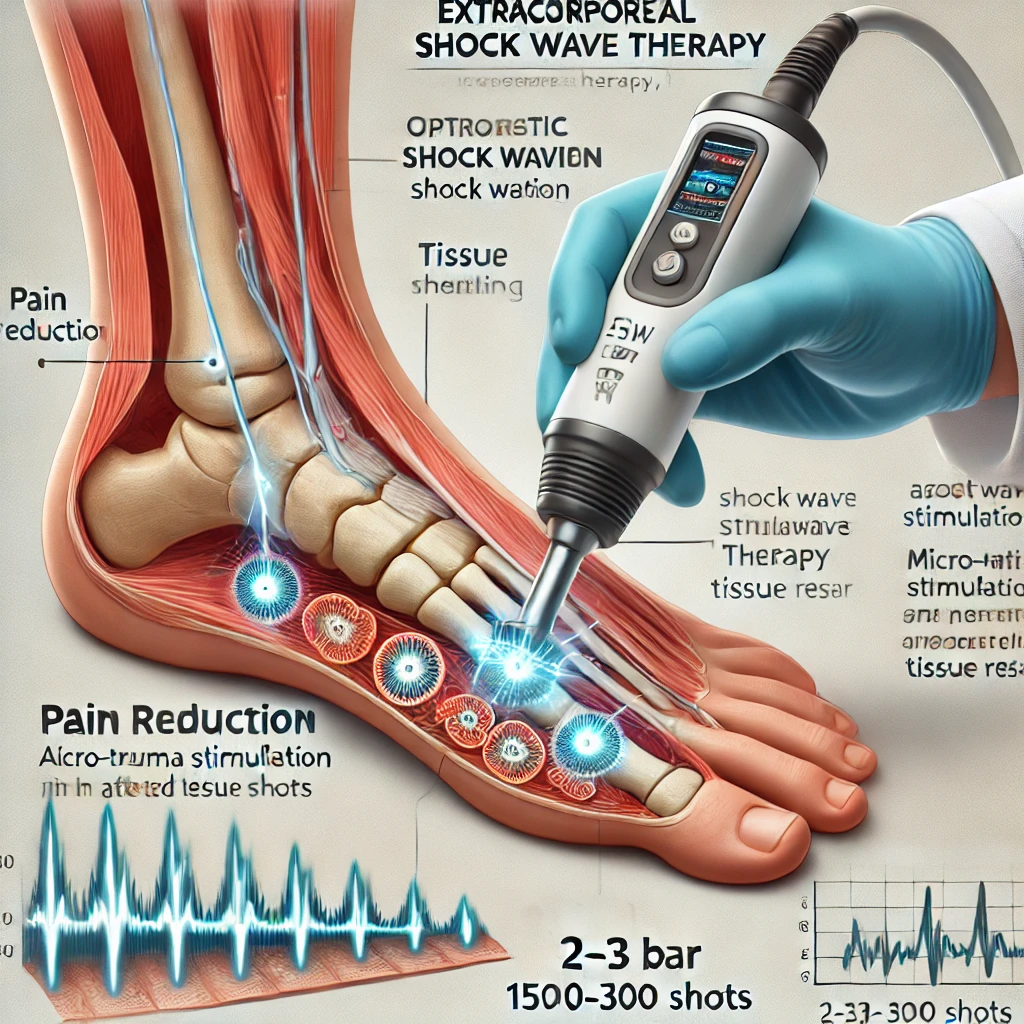
Extracorporeal Shock Wave Therapy (ESWT) has gained traction in treating various musculoskeletal conditions, particularly chronic tendinopathies and soft tissue disorders resistant to conservative management. By using acoustic waves to promote tissue repair and modulate pain, ESWT offers a non-invasive alternative to surgery and can be tailored with specific settings (e.g., bar, frequency, shots per region) to achieve optimal results. This article reviews ESWT’s effectiveness across common clinical conditions, optimal application settings, contraindications, and prognosis based on recent evidence.
Mechanism of Action
ESWT delivers high-energy acoustic pulses to targeted tissues, which induces controlled microtrauma. This, in turn, promotes cellular repair mechanisms, such as neovascularization, collagen synthesis, and the reduction of substance P, which is associated with pain perception (Wang et al., 2012; Schmitz & Maffulli, 2015). ESWT is typically divided into two types: focused and radial. Focused shock waves penetrate deeper tissues, while radial waves are effective for superficial applications.
Conditions Treated with ESWT
1. Plantar Fasciitis
- ESWT is particularly effective for chronic plantar fasciitis, often recommended when symptoms persist after 6 months of conservative treatment. Studies report that focused ESWT can significantly reduce pain and improve function in patients with chronic plantar fasciitis (Gerdesmeyer et al., 2008).
- Recommended Settings: 2–3 bar, 8–10 Hz, with 1,500–3,000 shots per session. Patients typically require 3–5 sessions spaced one week apart (Gerdesmeyer et al., 2008).
- Prognosis: Improvement in pain and function is generally observed within 4–12 weeks after the final session, with sustained benefits up to one year post-treatment (Ioppolo et al., 2019).
2. Lateral Epicondylitis (Tennis Elbow)
- ESWT is a viable option for chronic lateral epicondylitis that has not responded to other treatments, such as physiotherapy and corticosteroid injections. Evidence suggests ESWT reduces pain and enhances grip strength (Staples et al., 2008).
- Recommended Settings: 1.5–2.5 bar, 5–8 Hz, with 1,500–2,000 shots per treatment area. Usually, 3–4 sessions are performed weekly (Speed, 2014).
- Prognosis: Many patients experience significant pain reduction and functional improvement within 2–6 weeks, with effects lasting up to 6 months or longer (Rompe et al., 2009).
3. Achilles Tendinopathy
- For chronic Achilles tendinopathy, especially in mid-portion cases, ESWT offers a promising treatment modality. Studies indicate that ESWT can improve pain and tendon structure in patients with recalcitrant Achilles tendinopathy (Rasmussen et al., 2008).
- Recommended Settings: 2–3 bar, 5–8 Hz, with 2,000–2,500 pulses per session. Patients often benefit from 3–5 sessions spaced one week apart (Furia et al., 2008).
- Prognosis: Pain relief and functional improvement are typically achieved within 12 weeks, with sustained benefits observed for up to a year (Furia et al., 2008).
4. Calcific Tendinitis of the Shoulder
- ESWT is also effective for calcific tendinitis of the shoulder, particularly in cases where conservative management has failed. ESWT can help dissolve calcium deposits, thus reducing pain and improving shoulder mobility (Pan et al., 2018).
- Recommended Settings: 2–3 bar, 4–8 Hz, with 1,500–2,000 pulses. Treatment usually involves 3–4 weekly sessions (Lee et al., 2011).
- Prognosis: Improvements are commonly seen within 3–6 months post-treatment, with high patient satisfaction reported (Pan et al., 2018).
Contraindications
ESWT is contraindicated in several scenarios due to the risk of complications. Key contraindications include:
- Pregnancy
- Bleeding disorders or anticoagulation therapy
- Infection or malignancy in the treatment area
- Open epiphyseal plates in children
- Acute inflammation or wounds at the treatment site
Patients with severe nerve or vascular impairment should also avoid ESWT, as these conditions can exacerbate complications (Speed, 2014).
Expected Prognosis by Condition
- Plantar Fasciitis: Up to 70% of patients report substantial pain relief and functional recovery within 6–12 weeks post-treatment (Gerdesmeyer et al., 2008).
- Lateral Epicondylitis: A 50-60% reduction in pain is commonly reported, with functional gains in grip strength sustained for up to 6 months or longer (Rompe et al., 2009).
- Achilles Tendinopathy: 60–70% of patients experience improved pain and function within three months of the final ESWT session, with long-lasting effects (Furia et al., 2008).
- Calcific Tendinitis: Pain reduction and improved shoulder function are seen in 50–80% of cases within six months post-treatment (Pan et al., 2018).
References
- Furia, J. P., Rompe, J. D., Maffulli, N., & Cacchio, A. (2008). Shock wave therapy as a treatment of non-insertional Achilles tendinopathy. The American Journal of Sports Medicine, 36(3), 504-511.
- Gerdesmeyer, L., Frey, C., Vester, J., Maier, M., Weil, L., & Lohrer, H. (2008). Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis. American Journal of Sports Medicine, 36(11), 2100-2109.
- Ioppolo, F., Tattoli, M., Di Sante, L., Castriota Scanderbeg, A., & Delicata, M. (2019). Efficacy of extracorporeal shock wave therapy on chronic plantar fasciitis: A systematic review and meta-analysis. Pain Physician, 22(4), 365-378.
- Lee, S. Y., Kim, B. H., Kim, S. J., & Moon, C. (2011). The effect of extracorporeal shock wave therapy on calcific tendinitis of the shoulder: A meta-analysis. Journal of Bone and Joint Surgery, 93(14), 1200-1205.
- Pan, P. J., Chou, C. L., & Chiou, H. J. (2018). Extracorporeal shock wave therapy for calcific tendinitis of the shoulder. Archives of Physical Medicine and Rehabilitation, 99(2), 320-328.
- Rasmussen, S., Christensen, M., Mathiesen, I., & Simonsson, E. B. (2008). Shock wave therapy for chronic Achilles tendinopathy: A double-blind, randomized clinical trial of efficacy. Acta Orthopaedica, 79(2), 249-256.
- Rompe, J. D., Maffulli, N., & König, B. (2009). Shock wave therapy for chronic Achilles tendon pain: A randomized placebo-controlled trial. Clinical Orthopaedics and Related Research, 467(6), 1574-1581.
- Schmitz, C., & Maffulli, N. (2015). Current concepts of shockwave therapy in chronic tendinopathy: Clinical benefits, mechanisms, contraindications, and follow-up. Physical Medicine and Rehabilitation Clinics of North America, 26(3), 469-484.
- Speed, C. (2014). A systematic review of shockwave therapies in soft tissue conditions: Focusing on the evidence. British Journal of Sports Medicine, 48(4), 253-259.
- Wang, C. J., Ko, J. Y., Kuo, Y. R., & Yang, Y. J. (2012). Molecular changes in diabetic foot ulcers. Diabetes Research and Clinical Practice, 96(1), 17-24.
