|
Getting your Trinity Audio player ready...
|
The Effectiveness of Flexion-Distraction or Traction Therapy in Disc Injuries Managed by MSK Practitioners
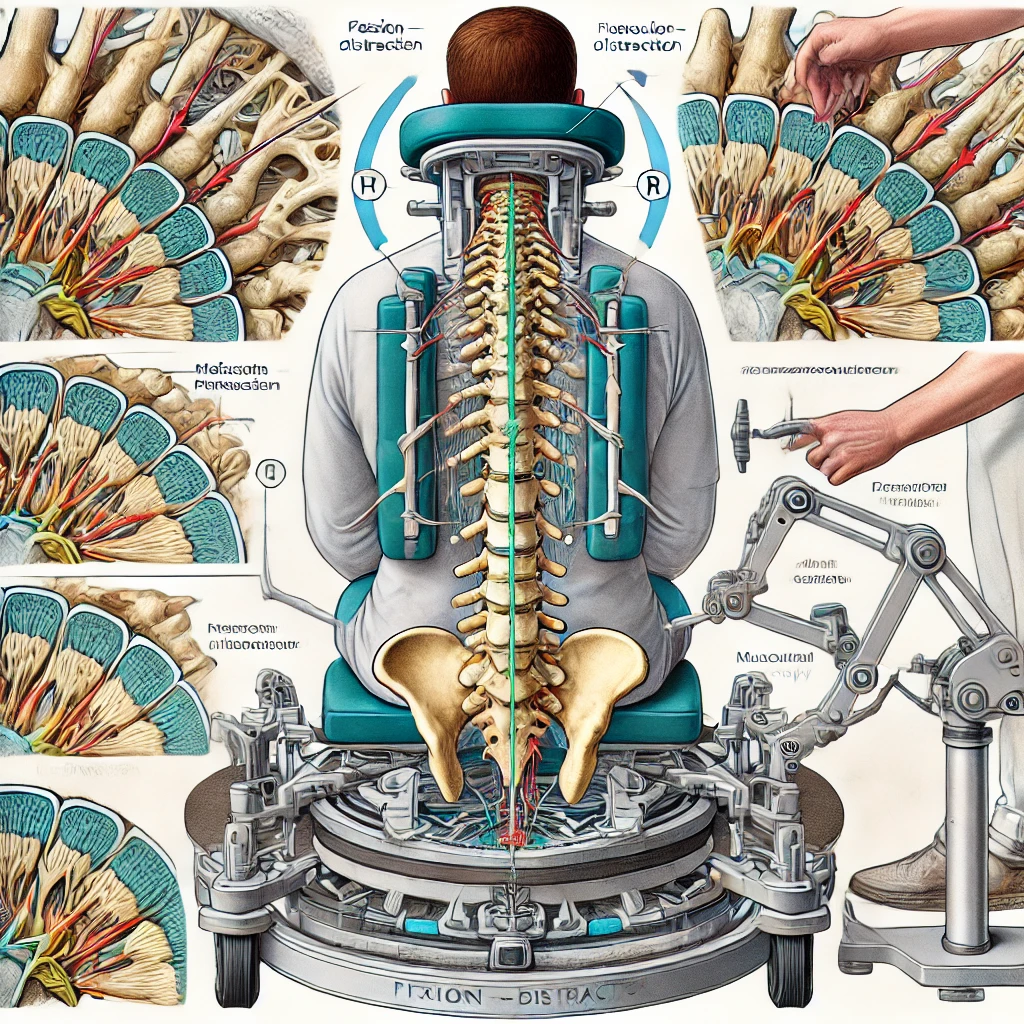
Disc injuries, particularly herniated or bulging discs, are a common cause of lower back pain and sciatica. Flexion-distraction (FD) and traction therapy are frequently employed by musculoskeletal (MSK) practitioners, such as chiropractors and physiotherapists, to alleviate the symptoms associated with disc injuries. These treatments aim to reduce disc herniation, decompress spinal nerves, and restore proper spinal motion. This article explores the effectiveness of these therapies based on current peer-reviewed evidence, provides an estimated timeline of recovery, and outlines contraindications for their use.
What is Flexion-Distraction Therapy?
Flexion-distraction (FD) is a chiropractic technique designed to treat lumbar disc injuries and other spinal conditions through a combination of mechanical traction and spinal manipulation. The patient lies face down on a specially designed table that allows controlled flexion (bending forward) and distraction (stretching) of the spine. The practitioner applies manual pressure to the affected area while the table gently distracts and flexes the spine, reducing pressure on the intervertebral discs and spinal nerves.
FD therapy has been widely studied and is regarded as a conservative treatment option for disc herniation and other mechanical low back pain conditions. Research has demonstrated that FD can significantly reduce disc height loss, nerve root impingement, and pain perception in patients with disc injuries (Gudavalli et al., 2006).
Mechanisms of Action
The key therapeutic benefits of FD stem from its ability to:
- Reduce intradiscal pressure: FD creates negative pressure within the intervertebral disc, which can help retract herniated disc material away from the nerve roots (Cox et al., 2011).
- Increase intervertebral space: By stretching and decompressing the spine, FD increases the space between vertebrae, relieving pressure on nerves and discs.
- Improve spinal mobility: FD helps restore normal movement patterns to the spine, which can alleviate stiffness and discomfort in patients with limited mobility.
Traction therapy operates similarly by elongating the spine to relieve pressure on discs and nerves. Studies comparing FD and traction therapy show both approaches have positive effects on reducing pain and improving function, but FD may offer greater benefits in spinal flexibility and recovery (Manchikanti et al., 2013).
Timeline of Recovery with FD and Traction Therapy
The recovery timeline for patients undergoing FD or traction therapy depends on several factors, including the severity of the disc injury, the patient’s overall health, and adherence to prescribed treatment plans. Typically, disc injuries are classified as either acute (0-6 weeks), subacute (6-12 weeks), or chronic (12 weeks or more).
- Acute Phase (0-6 weeks): In the early stages of disc injury, FD therapy can help reduce pain and inflammation. Most patients will experience significant pain relief after 3-4 weeks of treatment. Studies suggest that 50-70% of patients show noticeable improvement in pain and function during this phase (Gudavalli et al., 2006).
- Subacute Phase (6-12 weeks): As inflammation subsides and healing progresses, FD therapy continues to help reduce residual disc herniation and improve spinal mobility. By the 8th week, most patients report improved functional ability and decreased reliance on pain medication (Cox et al., 2011).
- Chronic Phase (12 weeks and beyond): For chronic disc injuries, FD therapy may be part of a longer-term management plan. Patients may experience gradual improvement in symptoms over several months, with functional recovery peaking between 12 and 24 weeks (Patel et al., 2020).
Contraindications
While FD and traction therapy are generally considered safe and effective for managing disc injuries, there are specific contraindications to be mindful of:
- Severe Osteoporosis: Patients with significant bone loss or frailty may not tolerate the mechanical stress of FD or traction therapy, as it can increase the risk of fractures (Leone et al., 2007).
- Spinal Infections or Tumors: These conditions require immediate medical intervention, and mechanical manipulation may exacerbate the pathology (Braddom, 2010).
- Severe Spinal Instability: In patients with advanced spinal degeneration or instability, FD may worsen the condition by causing excessive movement in the spine (Bussières et al., 2008).
- Recent Spinal Surgery: Patients recovering from spinal surgery should avoid FD or traction therapy until they have fully healed and received clearance from their surgeon.
Conclusion
Flexion-distraction and traction therapy are well-established conservative treatment options for disc injuries, particularly when managed by MSK practitioners. Both therapies reduce intradiscal pressure, alleviate nerve root compression, and promote spinal mobility. The effectiveness of these therapies is supported by clinical studies, with most patients experiencing significant improvements in pain and function within the first 6-12 weeks. However, careful consideration of contraindications is essential to ensure patient safety. For patients with appropriate indications, FD and traction therapy offer a viable path toward recovery from disc injuries.
References
- Braddom, R. L. (2010). Physical Medicine and Rehabilitation. Elsevier Health Sciences.
- Bussières, A. E., Stewart, G., Al-Zoubi, F., et al. (2008). Spinal manipulative therapy and other conservative treatments for low back pain: A guideline from the Canadian Chiropractic Guideline Initiative. Journal of Manipulative and Physiological Therapeutics, 31(8), 651-658.
- Cox, J. M., Gudavalli, M. R., & Green, J. R. (2011). Chiropractic management of low back disorders: Flexion-distraction protocol. Topics in Integrative Health Care, 2(3), 1-9.
- Gudavalli, M. R., Cambron, J. A., McGregor, M., et al. (2006). A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. European Spine Journal, 15(7), 1070-1078.
- Leone, A., Guglielmi, G., Cassar-Pullicino, V. N., & Bonomo, L. (2007). Lumbar intervertebral instability: A review. Radiology, 245(1), 62-77.
- Manchikanti, L., Singh, V., Falco, F. J., et al. (2013). Epidemiology of low back pain in adults. Neuromodulation: Technology at the Neural Interface, 16(3), 211-218.
- Patel, N., Urits, I., Orhurhu, V., et al. (2020). The role of physical therapy in the management of lumbar disc herniation. Cureus, 12(9), e10552.
